Which Contraception Is Best for Me? A South African Guide Based on Your Body, Health & Lifestyle
- Samantha Pieterse

- 10 hours ago
- 13 min read

Choosing contraception is important. And it’s complicated, but also it’s deeply personal. There isn’t one method that works for everyone. Your medical history, your cycle, your lifestyle, and your plans all shape what feels right and works well for you.
In South Africa, you have so many options. Short-term, long-term, hormonal, and non-hormonal, each with its own advantages and trade-offs.
So instead of searching for the “best contraceptive,” a better question is: Which option suits me best?
This guide breaks it down, so you understand your options and can make a decision that feels right for you.
What Does “Best Contraception” Actually Mean?
When someone asks for the “best contraception,” they usually mean one of three things: effectiveness, safety, or minimal side effects. The right contraceptive is the one that’s safe for your health profile and realistic for your routine.
Which Contraceptive Method Is Most Effective at Preventing Pregnancy?
Effectiveness refers to how well a contraceptive method prevents pregnancy. It’s usually described in two ways: perfect use, meaning the method is used exactly as instructed every time, and typical use, which reflects real-life scenarios such as missed pills, late injections, or condom mistakes. The difference between these two can significantly affect how reliable a method is in practice.
Long-acting reversible contraceptives are among the most effective options because they remove user error. Once inserted, they work continuously without requiring daily or weekly action. Shorter-acting methods like pills, patches, or injections can also be highly effective, but their reliability depends more heavily on consistent use.
Which Contraception Has the Fewest Side Effects?
Effectiveness is only one part of the decision. The other is side effects. Side effects vary between hormonal and hormone-free methods, and between individuals.
Hormone-free methods avoid hormone-related effects, but bleeding changes can still happen. Hormonal options may regulate cycles but can cause temporary adjustment symptoms in the first few months.
The goal is to choose a method where the benefits outweigh the downsides.
Is There a Safest Form of Birth Control?
There isn’t one single “safest” method for everyone. Safety depends on your individual medical history. Hormone-free options can be a good fit for some women, but they aren’t automatically safer across the board. They may suit those who prefer long-term protection without systemic hormonal effects and who are comfortable continuing with regular menstrual bleeding.
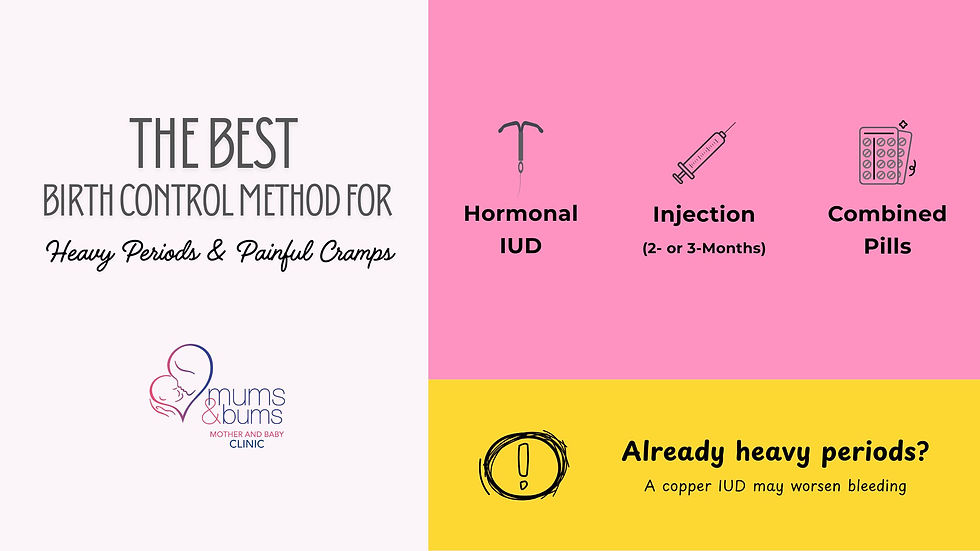
Best Contraception for Heavy Periods, Painful Cramps, or Anaemia
If your periods are heavy, painful, or leave you exhausted each month, contraception isn’t only about preventing pregnancy. It can also play a role in treatment. Heavy bleeding is more than an inconvenience. Over time, it can contribute to low iron and ongoing fatigue. The right method can significantly reduce bleeding and cramping, while the wrong one may worsen both. That’s why this is a decision where fit really matters.
Which Birth Control Helps Reduce Heavy Bleeding?
Some hormonal contraceptives thin the lining of the uterus, which usually results in lighter periods. Methods that often reduce bleeding include the hormonal IUD (such as Mirena), the contraceptive injection, and certain combined oral contraceptive pills. Many women notice shorter periods, lighter flow, less clotting, and fewer overall bleeding days.
In contrast, the hormone-free copper IUD can make bleeding heavier or cramps stronger, particularly in the first few months. That’s an important consideration if your periods are already challenging.
Can Contraception Help with Painful Periods?
Yes, especially if your pain is linked to strong contractions or heavy bleeding. Hormonal methods that reduce ovulation or thin the uterine lining often ease cramping, lessen pelvic pressure, and improve overall cycle control.
For women with conditions such as endometriosis or adenomyosis, certain hormonal options can also form part of longer-term symptom management. The goal isn’t simply to dull the pain each month, but to choose a method that addresses the underlying pattern driving it.
When Do Heavy Periods Need a Medical Check-Up?
While some women naturally have heavier cycles, certain patterns shouldn’t be dismissed. Book a review if your period regularly lasts longer than 7–8 days, you’re soaking through a pad or tampon every 1–2 hours, passing large clots most cycles, feeling persistently fatigued or dizzy, or bleeding between periods.
These signs don’t necessarily mean something serious is wrong, but they do deserve proper assessment before starting or changing contraception. In many cases, the right method can both prevent pregnancy and noticeably improve your cycle.
Best Contraception If You Forget to Take Pills
If daily medication isn’t your strength, there are still options. Daily pills work well, but only when taken consistently. Real life is busy, and missed tablets are one of the most common reasons contraception fails. If remembering medication feels stressful, a low-maintenance option may suit you.
What Is the Best Low-Maintenance Birth Control Option?
Low-maintenance contraception removes the daily mental load, making it easier to stay consistent without constantly thinking about it. It can be especially helpful if you travel often, work shifts, manage a busy household, struggle with routine medication, or simply prefer something discreet.
These options also often appeal to women who feel confident they don’t want a pregnancy for several years, whether that’s because their family is complete or because they’re simply not planning children anytime soon.
In South Africa, low-maintenance options include the contraceptive injection, the implant, and the IUD (hormonal or copper). Some last a few months, while others work for several years. All are highly effective because they don’t rely on daily action.
The right option depends on how long you want protection and whether you’re more comfortable with a once-off procedure or occasional repeat clinic visits.
Implant vs. IUD vs. Injection: What’s Easier to Manage?
All three are designed to reduce day-to-day responsibility, but they differ in how they’re maintained.
The implant is inserted under the skin of the arm and lasts up to 3 years with no routine follow-ups unless you have concerns.
The IUD is placed in the uterus during a clinic visit and can work for five to ten years, depending on the type.
The injection requires no procedure but must be repeated every 2 or 3 months.
Here’s how they compare:
Method | How It’s Given | How Long It’s Effective | Ongoing Maintenance |
|---|---|---|---|
Implant | A small rod is inserted under the skin of the arm. | Up to 3 years | None after insertion unless concerns arise |
IUD (Hormonal or Copper) | Inserted into the uterus during a clinic visit. | 5 years | No routine action required |
Injection | An injection that is given in the clinic. | 2 or 3 months | Requires repeat appointments |
There isn’t a universally easier option. The best option is the one that fits your comfort level and the amount of ongoing responsibility you want to manage.

Best Hormone-Free Contraception Options in South Africa
Some women know from the start that they would prefer to avoid hormones. Others have tried hormonal contraception before and didn’t feel like themselves on it. Wanting a hormone-free option narrows the available methods.
In South Africa, the main hormone-free long-term option is the copper IUD.
Is the Copper IUD the Only Hormone-Free Option?
For long-acting, highly effective contraception without hormones, the copper IUD is currently the primary option available.
It works by creating an environment inside the uterus that prevents fertilisation. It does not stop ovulation, and it does not contain oestrogen or progesterone.
Other hormone-free methods include:
Male or female condoms
Natural fertility awareness methods
Permanent sterilisation (for those certain about not wanting future pregnancies)
In terms of long-term, reversible, and highly effective contraception, the copper IUD is currently the main hormone-free option available. Because it doesn’t thin the uterine lining, some women notice heavier periods, stronger cramps, or slightly longer cycles, especially in the first few months, which is important to consider if your periods are already difficult. This is important if your periods are already heavy.
Who Should Consider Non-Hormonal Contraception?
Hormone-free contraception may suit women who prefer to maintain their natural cycle, have experienced significant hormone-related side effects in the past, or have medical conditions where certain hormones are not recommended. It can also appeal to those who want long-term contraception without systemic hormonal effects and who are comfortable continuing with regular menstrual bleeding.
Choosing hormone-free contraception is less about avoiding hormones and more about deciding whether the trade-offs will work for you.
If you’re unsure, a short review of your health history and menstrual pattern is usually enough to clarify whether hormone-free contraception is a good fit or whether a low-dose hormonal option may actually suit you better.

📍At Mums & Bums, we can look at your cycle, your history, and your plans, and help you tochoose a method that feels right for you.
Best Contraception If You Want to Fall Pregnant Soon
If you’re thinking about pregnancy in the near future, whether that’s in a few months or within a year, you need to factor fertility timing into your contraceptive choice. Most methods are reversible, but they don’t all return fertility at the same pace. Understanding what to expect can help you plan with less stress and fewer surprises.
How Quickly Does Fertility Return After Stopping the Pill or Patch?
For most women, fertility returns within a few weeks after stopping the pill or patch. Ovulation may resume by the first natural cycle, although periods can be slightly irregular at first.
How Long Does the Injection Stay in Your System?
The contraceptive injection can delay ovulation longer than other methods. Fertility often returns within several months, but in some women, cycles may take up to 9–12 months to normalise.
Does the IUD or Implant Delay Fertility?
Fertility usually returns quickly after removal of an IUD or implant, often within the first few weeks or cycle. Unlike the injection, these methods are not associated with delayed return to fertility.
There is no evidence that these methods cause long-term fertility problems. The main advantage is that they offer strong protection while in place, but once removed, your body can return to its natural cycle.
Comparison: Fertility Return After Different Methods
Method | When Fertility Usually Returns | What to Expect |
|---|---|---|
Pill or Patch | Often, within a few weeks | Ovulation may resume by the first natural cycle. Cycles can be slightly irregular at first, especially if they were irregular before starting the pill. |
Contraceptive injection | Commonly, within several months | Ovulation can take longer to restart. For some women, cycles may take up to 9–12 months to normalise. |
Hormonal IUD | Usually, within weeks after removal | Fertility often returns quickly once the device is removed. |
Copper IUD | Usually, within weeks after removal | Because it contains no hormones, ovulation typically resumes immediately once removed. |
Contraceptive implant | Often, within weeks after removal | Ovulation can resume as early as the first cycle after removal. |

Best Contraception If You Have Migraines
If you have migraines, contraception needs more careful selection because certain hormones can influence headache patterns. The key distinction isn’t simply “migraine or no migraine.” It’s the type of migraine you experience and whether you have neurological symptoms beforehand.
Can Hormonal Contraception Make Migraines Worse?
In some women, hormonal fluctuations can trigger or worsen migraines. This is most commonly linked to oestrogen-containing methods, particularly around the hormone-free interval in combined oral contraceptive pills.
Some women may notice:
Headaches worsening during pill-free days
More frequent migraines after starting a new method
Headaches linked to hormonal cycle changes
Others experience no change at all, and some even notice improvement if their natural hormonal swings are stabilised. If migraines worsen after starting a contraceptive method, it doesn’t mean the method is unsafe, but it may mean an adjustment is needed.
Which Birth Control Is Safer If You Have Migraines With Aura?
Migraines with aura (where you have temporary visual, sensory, or speech changes before the headache) are treated differently from migraines without aura in medical guidelines. In women with migraines with aura, oestrogen-containing contraceptives are generally not recommended due to an increased risk of stroke.
Safer options include:
The progestogen-only pill
The contraceptive injection
The implant
Hormonal IUD
Copper IUD (hormone-free)
Having migraines does not remove your contraception choices. It simply narrows down a little. A brief review of your migraine history is usually enough to identify which methods are suitable and which are better avoided.

Best Contraception for Women Who Smoke or Vape (Especially Over 35)
Smoking/vaping influences which contraceptive methods are considered safest. This becomes especially important after age 35, when cardiovascular risk naturally increases. If you only smoke occasionally, that doesn’t automatically rule out certain options, but it’s still important to mention it. Contraception safety is about the full context.
Why Combined Pills May Not Be Suitable If You Smoke
Combined oral contraceptive pills contain oestrogen. Oestrogen slightly increases the risk of blood clots, stroke, and heart complications. Smoking also increases these risks, and so the combination of the two raises concern further, particularly in women over 35.
Medical guidelines generally advise against using oestrogen-containing contraception if you:
Smoke and are over 35
Have high blood pressure
Have a history of blood clots
Have certain cardiovascular risk factors
Safer Contraception Options for Smokers
For women who smoke, especially over 35, options without oestrogen are typically preferred. These may include:
The progestogen-only pill
The contraceptive injection
The implant
The hormonal or copper IUD
These methods do not carry the same clot-related risk as combined pills.
If you smoke (even occasionally) and are considering contraception, let your provider know, so that they can choose the safest possible option for your current health profile. There are still several suitable and effective choices available.

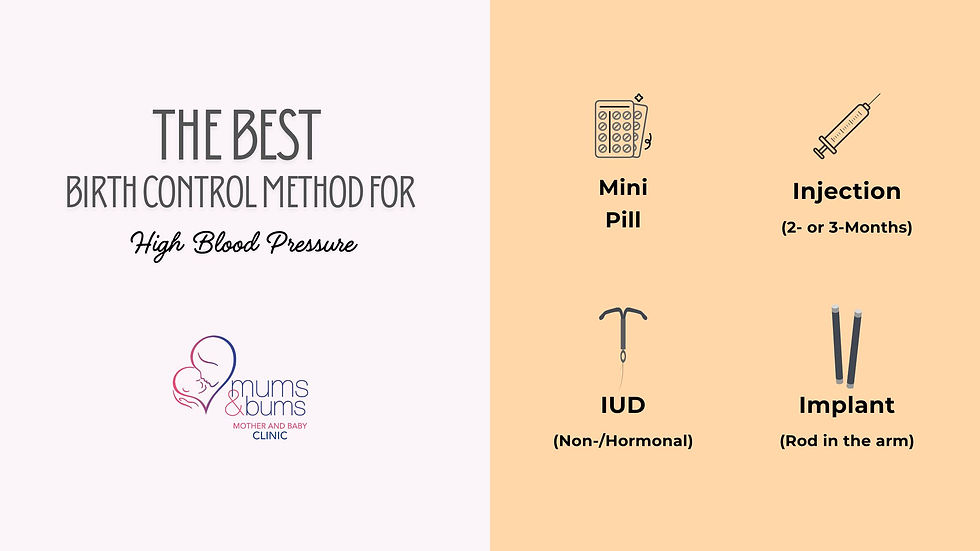
Best Contraception If You Have High Blood Pressure
If you have high blood pressure, even if it’s controlled, contraception needs more careful selection. This is because some methods contain oestrogen, which can slightly raise blood pressure and increase the risk of blood clots or stroke in women who already have cardiovascular risk factors.
Combined methods, such as certain oral contraceptive pills and the patch, are usually not recommended if your blood pressure is persistently elevated or if you are on treatment for hypertension.
The good news is that many safe options remain available. Methods that do not contain oestrogen, such as the progestogen-only pill, the injection, the implant, the hormonal IUD, or the copper IUD, are generally preferred in women with high blood pressure.
Having hypertension doesn’t remove your choices. It simply shifts the focus toward methods that protect you without increasing cardiovascular risk. A quick blood pressure check and brief review of your history is often all that’s needed to identify a suitable and safe option.
Best Birth Control for Acne, Mood Changes, or Weight Concerns
For many women, contraception isn’t only about preventing pregnancy, but also about how it makes you feel in your skin and in your body. Concerns about acne, weight, and mood are common. The key is understanding what is evidence-based, what varies among individuals, and which options are more predictable.
No contraceptive is completely free of potential side effects, but some patterns are clearer than others.
Which Birth Control Can Help With Acne?
Acne is closely linked to hormones, so it makes sense that contraception can sometimes influence your skin (mostly for the better).
Certain combined oral contraceptive pills are known to improve acne because they help balance hormone fluctuations and reduce the oil production that contributes to breakouts. For some women, this can mean fewer pimples, less inflammation, and clearer skin over a few months.
Not all methods have the same effect, though. Progestogen-only options don’t usually improve acne and, in some women, may make breakouts slightly worse. If your skin is already a sensitive area for you, it’s worth mentioning it upfront when choosing contraception. That way, your method can support your skin while also preventing pregnancy.
Does Contraception Cause Weight Gain?
Weight gain is one of the most common concerns when choosing contraception. But most modern contraception options have not been shown to cause significant long-term weight gain. Some women notice temporary changes in the first few months, often related to fluid retention rather than true fat gain.
The injectable contraceptive has been linked to weight gain in some women, particularly with longer-term use, but this does not happen to everyone. Other methods, including IUDs and the implant, are not consistently associated with meaningful weight change.
If weight gain is an important factor for you, it’s worth discussing your personal history and previous experiences rather than assuming all contraception affects the body in the same way.
⚖️ If weight changes are a major concern for you, we’ve written a detailed breakdown on contraception and weight gain here.
Can Birth Control Affect Your Mood or Mental Health?
Hormones influence the brain, so, understandably, some women notice mood changes after starting hormonal contraception.
Possible experiences may include:
Increased irritability
Lower mood
Anxiety changes
Many women experience no mood changes at all. Some even feel more stable once cycle-related hormonal swings are reduced.
If you have a history of depression or anxiety, that doesn’t always mean that you will not be able to use hormonal contraception. It does, however, mean your response should be monitored more closely. The most important thing is recognising patterns. If mood changes begin after starting a method and persist, let your provider know so adjustments can be made.

Which Contraceptive Method Is Most Recommended in South Africa?
There isn’t one single method that’s “most recommended.” In South Africa, several contraceptive options are safe, effective, and widely used. The right choice depends on your health history, bleeding pattern, lifestyle, and pregnancy plans.
Instead of asking which method is best overall, it’s more useful to understand how the main options differ and which one fits you.
Is There a “Healthiest” Form of Birth Control?
There is also no one “healthiest” method. For example, women with migraines with aura are advised to avoid oestrogen-containing methods. Smokers over 35 are usually guided away from combined pills. Women with heavy periods may benefit from methods that reduce bleeding, while those wanting to avoid hormones may prefer non-hormonal options.
All approved contraceptive methods in South Africa are considered safe when appropriately matched to the user. The right method is the one that fits your body, minimises risk, and provides reliable protection.
When Should You Book a Contraception Review?
Most contraception decisions aren’t urgent, and a review doesn’t mean you need to start over. A review is just about making sure your current method is still healthy, and your plans are on track.
If side effects haven’t settled after a few months, bleeding feels heavier than expected, spotting is ongoing, mood changes have developed, migraines are worsening, or weight changes concern you, it’s reasonable to reassess. The same applies if you’re planning a pregnancy within the next year, have recently stopped a method, or your medical history has changed.
Contraception should evolve as you do. If you’re unsure whether your current method still fits, booking a contraception review can provide reassurance.
Frequently Asked Questions About Choosing Contraception
Which contraception is best for me?
The best contraception for you depends on your health history, menstrual pattern, lifestyle, and pregnancy plans. Some women prefer long-term, low-maintenance options like an IUD or implant, while others prefer pills or injections. A brief review helps match the method to your body and routine.
What birth control has the least side effects?
No contraceptive is completely side-effect-free, but many women tolerate modern methods very well. Side effects vary depending on whether the method contains hormones and how your body responds. Hormone-free options avoid hormonal effects, while low-dose hormonal methods may reduce cycle-related symptoms. The “least side effects” option differs between individuals.
What is the safest contraceptive method?
For most healthy women, several contraceptive methods are considered safe. But the safest option depends on personal factors such as smoking status, migraines, blood pressure, and medical history. Methods without oestrogen are often preferred for women with higher cardiovascular risk. Safety is individual, not one-size-fits-all.
Which contraception is best for heavy periods?
Hormonal methods that thin the uterine lining, such as the hormonal IUD, injection, or certain pills, often reduce heavy bleeding and cramping. The copper IUD may increase bleeding in some women. If heavy periods are causing fatigue or affecting daily life, choosing a method that lightens flow can be beneficial.
Can smokers take birth control pills?
Smokers under 35 without other risk factors may be able to use certain pills. However, combined pills containing oestrogen are generally not recommended for women over 35 who smoke due to increased cardiovascular risk. Progestogen-only methods or non-hormonal options are usually safer alternatives.
How soon can I get pregnant after stopping contraception?
Fertility usually returns quickly after stopping the pill, implant, or IUD, often within weeks. After the injection, ovulation may take several months to resume. Most methods do not cause long-term fertility delay, but timelines can vary between individuals.
Is hormone-free birth control better?
Hormone-free contraception is not necessarily better. It simply avoids hormonal side effects. In South Africa, the copper IUD is the main long-term hormone-free option. It suits women who prefer natural cycles but may increase bleeding or cramps in some cases. The best choice depends on your priorities.
Which birth control is most effective in South Africa?
Long-acting methods like the IUD and implant are among the most effective because they don’t rely on daily action. Pills and injections are also highly effective when used correctly. Effectiveness depends on both the method and how consistently it is used.



















Comments