Mirena® Birth Control: Benefits, Risks & What to Expect from the Hormonal IUD
- Samantha Pieterse

- Jul 31, 2024
- 8 min read
Updated: Sep 19, 2025
The Birth Control Revolution
The contraceptive revolution started in the 1960s. Suddenly, women were able to delay, space, and avoid pregnancies. Birth control has been life-saving for us as women. It is one of the most affordable and empowering inventions, and we at Mums & Bums are here to support it.
A Brief History of Contraception

The Mirena® is a stand-out option thanks to incredible advancements in contraceptive management. Because it is a long-term option that requires minimal maintenance, the benefits include nearly 100% effectiveness, long-term protection, and regulation of your period (or, in some cases, no period at all).
If You’re Comparing Birth Control Options
Check out our guide on the different types of birth control pills in South Africa or learn about the copper IUD as a hormone‑free alternative.
What is the Mirena® Intrauterine Device?
So, I’m sure you're wondering, “What is the Mirena®?” The Mirena® is a T-shaped plastic device inserted into your uterus. It works by releasing a steady stream of hormones into your system that can prevent pregnancy for up to 7 years.
How Does The Mirena® Prevent Pregnancy?
The Mirena® works in a few ways. Firstly, it thickens the mucus in your cervix, which prevents sperm from reaching the egg and fertilizing it. Secondly, it thins out the lining of your uterus so that if an egg were to be fertilized, it would not be able to implant. Lastly, the hormones in Mirena® prevent the release of an egg, a process known as ovulation. This means that your body will not release eggs for fertilization.
The Benefits of The Mirena® Birth Control
There are so many benefits to using this as a method of contraception:
The Mirena® is effective for up to 7 years. This means if you have completed your family, the Mirena® is an excellent option for a long-term contraceptive until you reach menopause.
It is convenient. Unlike the pill, which you need to remember to take at the same time each day and need to collect once a month, when the Mirena® is placed, it is effective for 7 years. The only maintenance required from your side is to check that you can feel the strings once a month after your period.
There is a lower risk of pregnancy due to your error because once it is in, you don’t need to remember anything except for string checks and replacing it every 7 years.
There are also some non-contraceptive benefits, such as possible reduction in menstrual bleeding and cycle regulation.
Who Can Use Mirena®?
Almost all women are suitable candidates for the Mirena®, but if you have the following, you may benefit even more from having the Mirena® placed:
Heavy bleeding during periods
Severe pain or cramping during periods
Endometriosis
Anaemia
Fibroids
We often discuss Mirena® birth control as an option during postnatal contraception planning, especially for new moms who are breastfeeding.
Who Can't Use the Mirena®?
As with any medical option, this is not suitable for everyone. If you have any of the following, you may better benefit from another contraceptive option:
Have or have had breast cancer
Have or have had uterine or cervical cancer
Liver disease
Fibroids that hinder the placement of the Mirena
Pelvic infection or pelvic inflammatory disease
Atypically shaped uterus
Migraines
Blood clotting disorders
Mirena® Insertion: What to Expect
Consultation for the Mirena®
During your visit, we will discuss whether Mirena® is the right contraceptive method for you. You are welcome to use this opportunity to ask questions and address any concerns.
Medical History: We will ask you questions about your medical history, including any previous pregnancies, details of your menstrual cycle, and any medical conditions or allergies you may have.
Pre-Insertion Preparation
The timing of the insertion can be important. While we don’t mind where you are in your cycle, it may be more comfortable to schedule the insertion during your period. This is because your cervix is naturally more open, making the process easier and less painful.
Medications: We suggest taking a pain reliever (like ibuprofen) an hour before the appointment to help manage discomfort during and after the procedure.
Arrival: Arrive at your appointment early to complete any necessary paperwork and relax before the procedure.
The Insertion Procedure
Examination: We perform a pelvic exam to check the position and size of your uterus and cervix.
Positioning: You’ll lie on the bed with your legs bent at the knees and your feet flat on the bed, similar to a pap smear.
Cleaning and Numbing: A speculum will be inserted so that we can see your cervix; this is a device that is used to open the vagina (in the same way that is done during a pap smear. We then clean your cervix and apply a numbing gel to minimize discomfort.
Measuring the Uterus: We will use a small instrument to measure the depth of your uterus, ensuring the proper placement of the Mirena®.
Inserting the Device: The Mirena® IUD, a small T-shaped device, is inserted through the cervix and into the uterus using a thin, flexible tube. During this part of the process, you may feel some cramping or discomfort.
Final Adjustments: The provider will trim the strings of the IUD to about 2-3 cm, which you’ll be able to feel high in your vaginal canal.
I know this all sounds very scary, but at Mums & Bums, we really strive to make this appointment as quick and comfortable as possible. The entire procedure takes no more than 5 minutes, including a Pap smear if necessary.
Post-Insertion Care
Rest and Recovery: After the insertion, you might experience cramping and spotting. Rest and use over-the-counter pain relievers as needed.
Follow-Up Appointment: Schedule a follow-up visit 6 weeks after the IUD insertion to ensure it is properly placed and to address any concerns.
Mirena® Removal: What to Expect
Consultation for the Mirena® Removal
During your visit: We will discuss the removal of your Mirena® IUD. Whether you’re planning to switch birth control methods, trying to conceive, or approaching the end of its effective period, this is the time to share your reasons and ask any questions.
Medical History: Please inform us of any changes in your health or reproductive plans since the insertion of your Mirena.
Pre-Removal Preparation
The timing of the removal can be flexible. Let us know the best time for you, especially if you're planning to switch contraceptives or trying to conceive.
Medications: We suggest taking a pain reliever (like ibuprofen) an hour before the appointment to help manage discomfort during and after the procedure.
Arrival: Arrive at your appointment early to complete any necessary paperwork and relax before the procedure.
The Removal Procedure
Positioning: You’ll lie on the bed with your legs bent at the knees and your feet flat on the bed, similar to a pap smear.
Locating the Strings: We will use a speculum to open your vagina and locate the IUD strings.
Gentle Removal: By gently pulling on the strings, the IUD’s arms will fold up as it slides out of the uterus through the cervix. This part of the process usually only takes a few seconds and may cause mild discomfort or cramping.
Final Check: We will ensure the entire device has been removed and check for any signs of complications.
Post-Removal Care
Immediate Aftercare: You might have some light spotting and mild cramping after the removal. Rest and use over-the-counter pain relievers as needed.
Monitoring Symptoms: Pay attention to your body’s response over the next few days. Light spotting and mild cramping are normal, but if you experience severe pain or heavy bleeding, contact your healthcare provider.
Common Myths and Misconceptions About The Mirena®
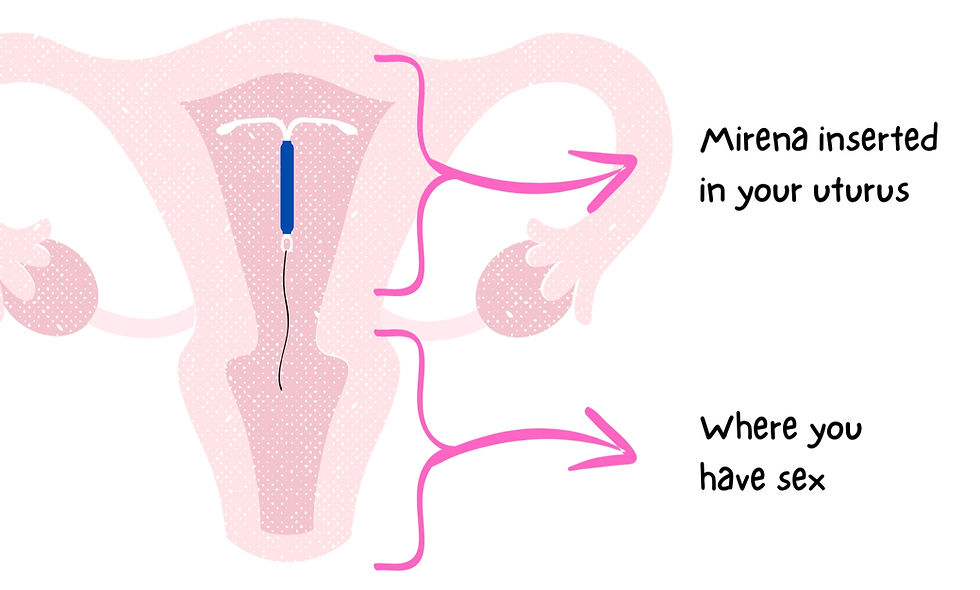
Myth 1: My partner will be able to feel the device during intercourse.
Fact: Intrauterine devices such as the Mirena® are inserted into the uterus, which is much higher up than where you will be having intercourse (vagina).
Myth 2: Women who have never been pregnant may not get a Mirena®.
Fact: Not having a previous pregnancy is not a contraindication for the Mirena®. This may be a great option for many women, regardless of whether you have been pregnant before.
Myth 3: The Mirena® is not safe. Many women have babies who are born with the Mirena in their hands.
Fact: While there is no one method that is 100% effective in preventing pregnancy, intrauterine devices such as the Mirena® and Copper-T are the number one most effective contraception methods. Less than 1% of women with an intrauterine device become pregnant while using this method.

Comparing The Mirena® to Other Birth Control Options
Method | Effectivity | Effective Time | Effect on Period | Ease of Use |
|---|---|---|---|---|
>99% | 3 – 5 years | It may take your period away completely | 4/5
No additional effort is required besides string checks. | |
Copper T/Loop | >99% | 7 – 10 years | No effect on your period | 4/5
No additional effort is required besides string checks. |
Implant | 99% | 3 years | May take your period away completely | 5/5
No additional effort is required. |
Injection | 96% | 2 or 3 months | It may take away or greatly reduce your period | 4/5
No additional effort is required. However, you must attend the clinic every 2 – 3 months to receive the injection. |
Pill | 92% | Monthly (or daily – it’s not effective if you miss one) | It may help to regulate your period. | 1/5
You need to remember to take it at the same time each day. |
Patch | 91% | Weekly (needs to be changed for it to be effective) | It may help to regulate your period. | 3/5
You need to change it weekly, but you don’t need to remember to do it each day. |
Condoms | 98%
If used correctly | One sex act | None | 0/5
It needs to be used correctly each time. |
Pull Out Method (Coitus-Interruptus) | 80% | One sex act | None | 0/5
It can be risky if not done in time. |
FAQs South African Women Ask About the Mirena®
What is the Mirena® IUD and how does it work?
The Mirena® is a small, T-shaped intrauterine device (IUD) placed in the uterus. It slowly releases a hormone (levonorgestrel) that prevents pregnancy by thickening cervical mucus, thinning the uterine lining, and sometimes stopping ovulation.
How long does the Mirena® last?
Mirena® provides birth control for up to 5 years. After that, it needs to be replaced if you want to continue using it.
What are the benefits of Mirena®?
Mirena® is more than 99% effective at preventing pregnancy. It can also make periods lighter, reduce cramps, and in some cases stop periods altogether.
What are the possible side effects or risks of the Mirena® IUD?
Some women experience irregular bleeding, headaches, breast tenderness, or mood changes at first. Rare but serious risks include infection or the IUD moving. Always discuss your medical history with a healthcare provider.
How much does Mirena® cost in South Africa?
Costs vary depending on the pharmacy and clinic. In South Africa, the Mirena® device itself usually ranges between R4000.00 and R5000.00, with additional fees for consultation and insertion.
Who should not use the Mirena®?
Mirena® is not suitable if you have certain uterine abnormalities, active pelvic infections, unexplained vaginal bleeding, or hormone-sensitive cancers.
Can I get pregnant after removing Mirena®?
Yes. Fertility typically returns quickly once Mirena® is removed, and many women can conceive within a few months.
Does Mirena® protect against sexually transmitted infections (STIs)?
No. Mirena® only prevents pregnancy. You’ll still need condoms to protect against STIs.
So, Is Mirena® Right for You?
Whether Mirena® birth control is right for you depends entirely on you. Contraception is not a one-size-fits-all approach. Each of your circumstances and issues needs to be considered before choosing the method you want to try.
Make an appointment at Mums & Bums today, and we will walk you through your options.
Still Unsure About Mirena®?
Book a family planning consultation at Mums & Bums and talk through your options with a nurse‑midwife who knows you and your health history.

















Comments